-
Posts
682 -
Joined
-
Last visited
Content Type
Forums
Profiles
Store
Gallery
Articles
Blogs
Events
Downloads
Posts posted by Dr. Carlos Wesley
-
-
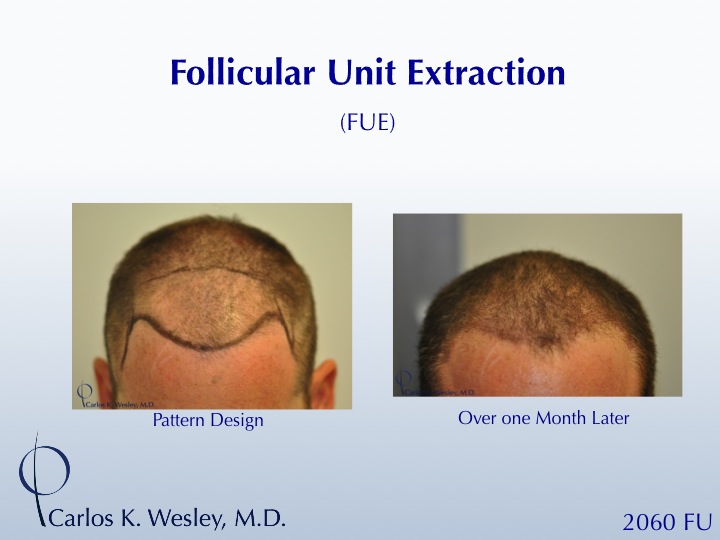
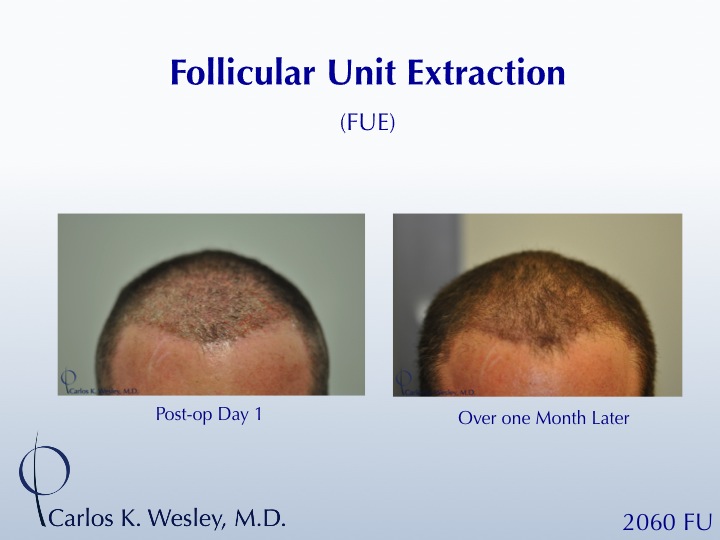
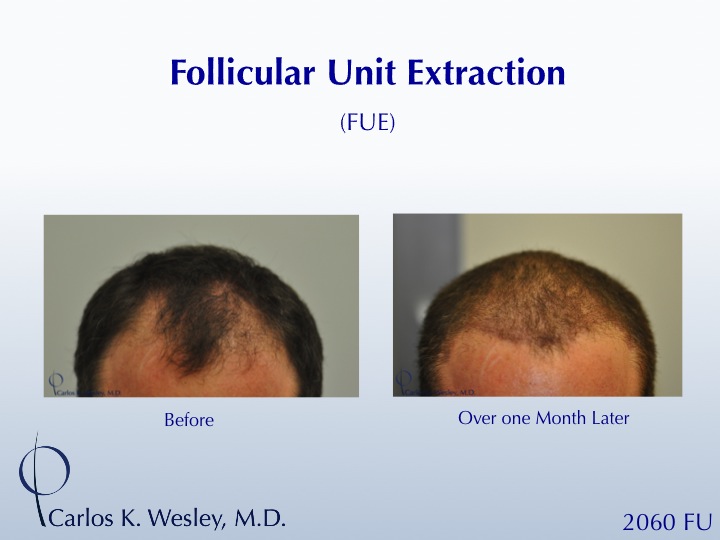
Here's a rather interesting finding over the past year in our office that I thought I would share with the community. Although it's purely anecdotal at this stage, I have observed that when incubated in platelet-rich plasma (PRP) and ACell during their out-of-body time, transplanted hair follicles appear less likely to shed early in the postoperative process.
For illustration, here is an FUE patient of mine who, in one day, had 2060 FU transplanted throughout his frontal half. He returned over a month later (a period before which micro graft shaft shedding had occurred in years past) and very few (if any) of the transplanted hair shafts had fallen out. This provided an early framing of this patient's face as the transplanted hair length closely matched that of his surrounding pre-existing hairs.
An observation that our office will certainly explore in more detail...
-
Thanks, Nick.
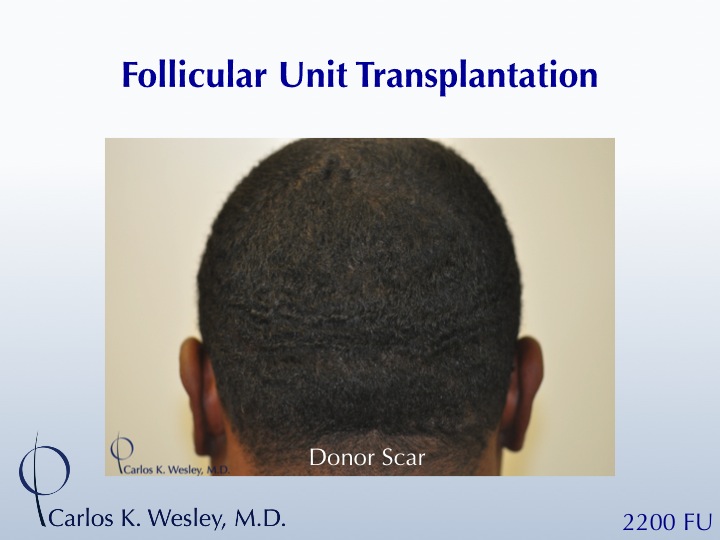
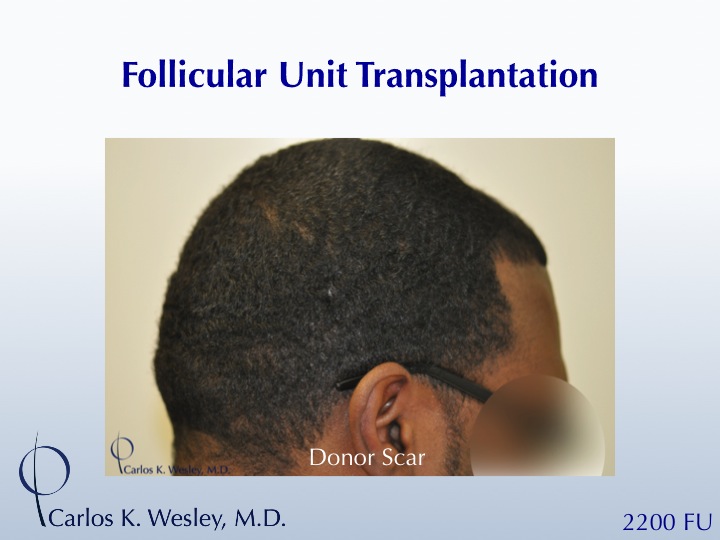
It's the minimal color contrast between the color of hair and color of scalp combined with the "shingling" effect of having curly hair that can give African-American patients the illusion of more coverage with fewer grafts. I've encouraged this patient to wear his hair a few millimeters longer in order to take advantage of this "shingling" effect. But, he is just happy to be able to continue to wear his short hairstyle even after a strip harvest (FUT or FUSS).
-
Thanks, Jotronic, for your reply. It certainly makes for an interesting topic of discussion.
While every clinic differs slightly in their approach and what works best in their hands, a point of clarification that I think is important not to gloss over is the essential shape of the grafts prior to transplantation. There should, therefore, be a limit to the degree of graft trimming.
The "Hair Transplantation" textbook has, for many years, stated that:
"The 'perfect' follicular unit graft (is that possessing) very little dermis, sufficient subcutaneous fat, intact sebaceous gland, and an overall pear shape."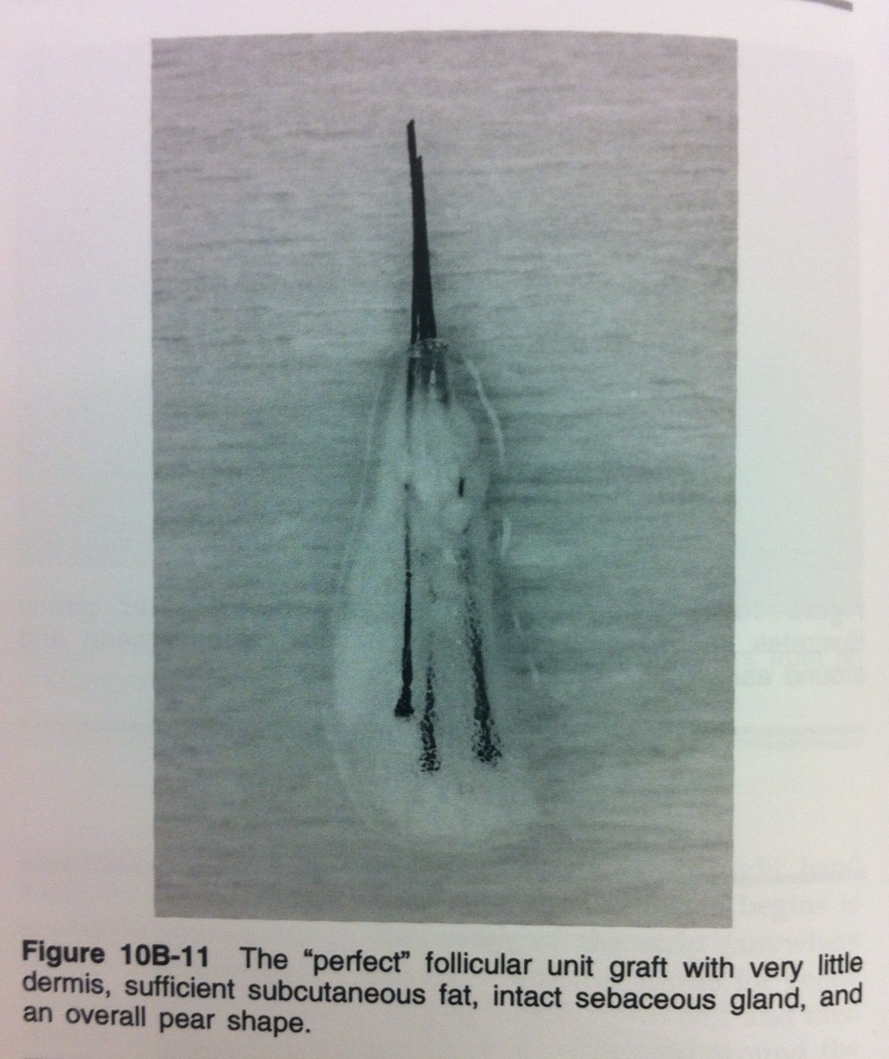
Leaving ample protective tissue around the infundibulum and dermal papilla (stem cell-containing portion of the hair follicles) shields the grafts from various environmental hazards while they are out of the body (e.g. desiccation and the trauma of being handled when transplanted). The amount of tissue has been shown to directly impact the survival of grafts in numerous studies (Dr. Michael Beeher's "surrounding tissue" study, Dr. Seager's viability study, and Dr. Greco's "crush study").[1,2,3]
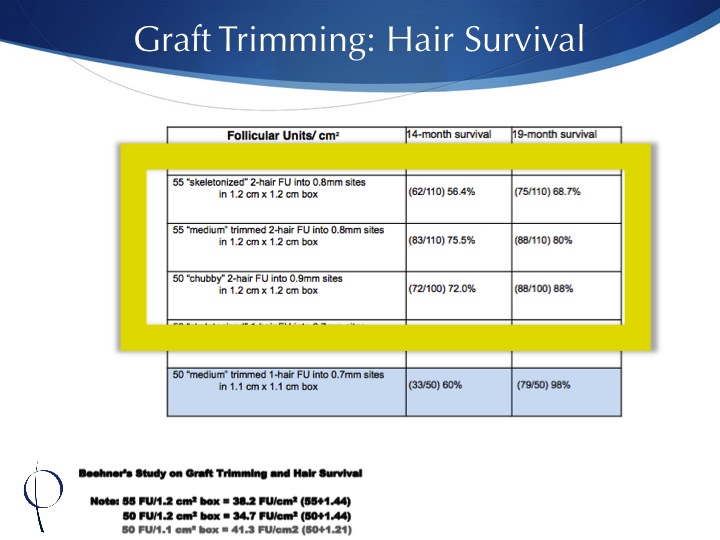
Looking at Beehner's study (below) we see how the amount of protective tissue does influence graft survival (especially at 19 months postoperatively).
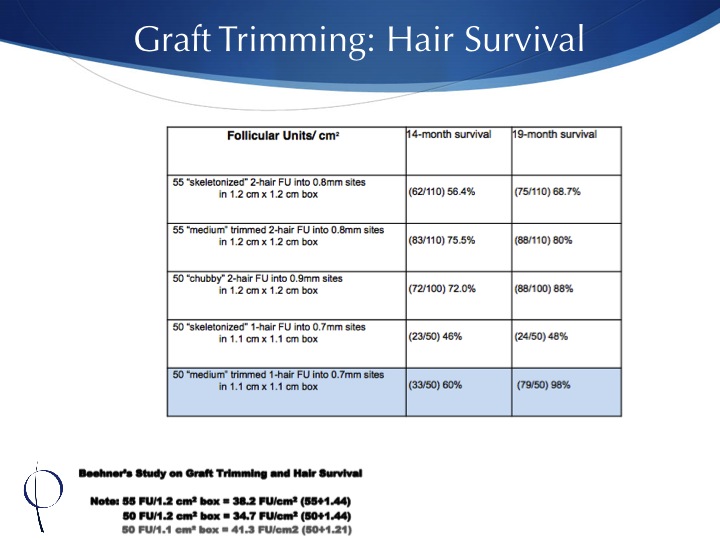
To better understand this investigation, let's focus on the grafts of the same type. So, two-haired grafts, for example, differ mainly in the amount of tissue surrounding them: from "skeletonized" (significantly trimmed) to "chubby" (not markedly trimmed). That's a 129% difference in graft survival at 19 months (see below).
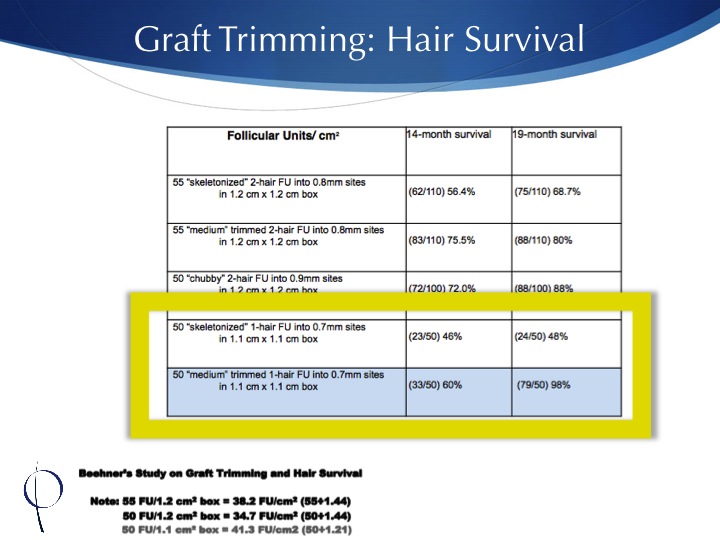
Now, when we focus on one-haired follicles (which are more commonly used in the hairline of patients), the difference in transplanted hair survival is even more pronounced (see below). Dr. Beehner showed a 204% difference in hair survival when the grafts were trimmed to a skeletonized shape versus their "chubby" counterparts.
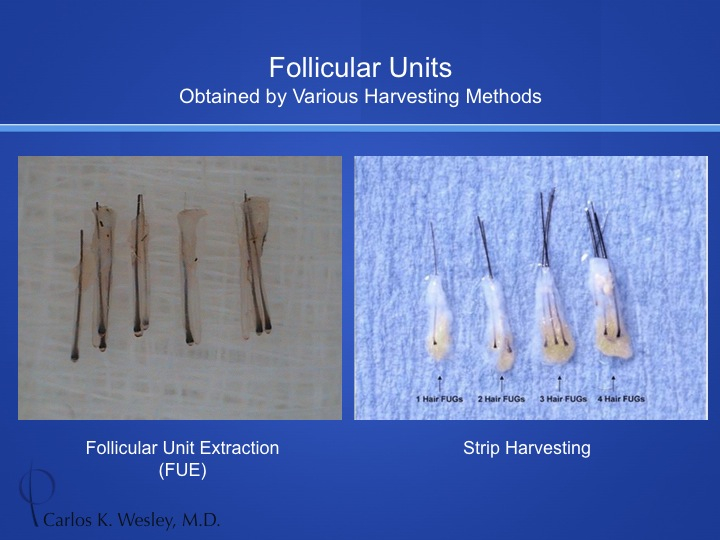
Why does this matter? And how does this relate to my initial posting? Well, the beauty of strip harvest (FUT or FUSS) grafts is the amount of surrounding tissue that can be included in each graft to ensure the greatest survival of transplanted follicles (see below). Trimming that to an advanced degree in order to pack them into sites that may not be able to accommodate grafts with more protective tissue may have the aforementioned detrimental effect on their ultimate survival. Now, while the general lack of protective tissue of FUE grafts is not necessarily advantageous, it may allow the grafts to more easily fit into more closely packed recipient sites.
Fortunately, Jotronic, you are representing an excellent surgical clinic with skilled physicians and technicians. So, these reproduced findings may not hold true in patients with whom you have dealt. I do feel, however, that these findings are important to point out.
- Beehner M. A comparison of hair growth between follicular-unit grafts trimmed “skinny” vs. “chubby.” Hair Transplant Forum Int 1999;9:16.
- Seager DJ. Micrograft size and subsequent survival. Dermatol Surg 1997; 23:757-61.
- Greco JF, Kramer RD, Reynolds GD. A crush study review of micrograft survival. Dermatol Surg 1997;23:752-5.
- Beehner M. A comparison of hair growth between follicular-unit grafts trimmed “skinny” vs. “chubby.” Hair Transplant Forum Int 1999;9:16.
-
@scar5:
Propecia may delay the onset of miniaturization because it slows down the cycling of hair follicles. With each cycle, hair follicles may become progressively finer in caliber.
@ali1991:
There are a number of methods to evaluate hair characteristics. Any physician performing surgical hair restoration likely has something to accurately analyze hair quality in order to determine a patient's candidacy. There are instruments such as the Folliscope, the FotoFinder device, the Dermatoscope, etc. A magnified lens allows for fairly accurate analysis. If you happen to have (a whole lot of) time on your hands, you can read the chapter I authored in the Hair Transplantation textbook called "Enhanced Patient Selection: The Folliscope".*
@RecedingTide:
Yes. Propecia is a great adjunct to surgery. Since it is most effective in the crown and mid scalp, it allows for a surgical focus on the frontal half of the scalp and a medical approach on the remaining portions. This can certainly delay the need for subsequent sessions to those areas. Remember, though, once a patient stops taking the medication, any benefit they received is lost. So, it's essential that areas of future loss are also addressed with any surgical approach to transplanting hair follicles.
*Wesley CK. "Enhanced Patient Selection: The Folliscope" Hair Transplantation, 5th Ed., Ungers and Shapiro: 82-83. 2011
-
Thanks, everyone, for your comments.
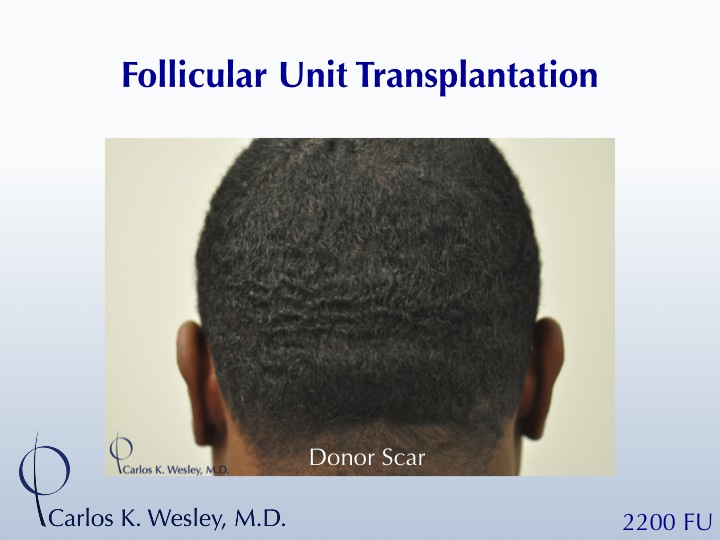
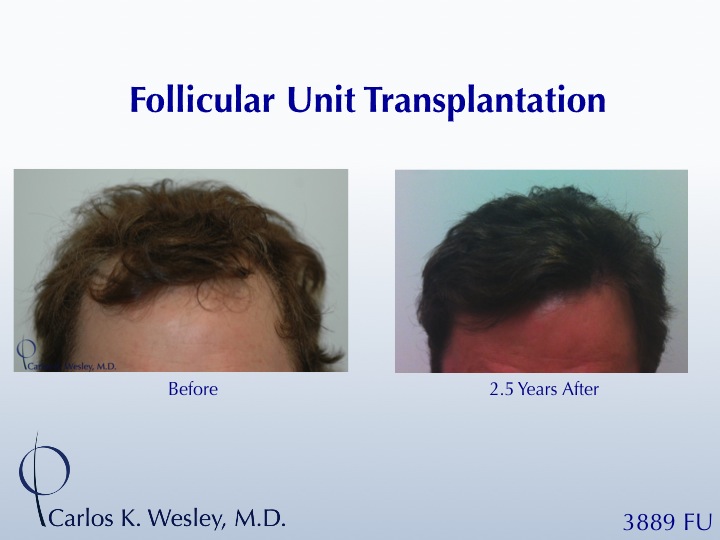
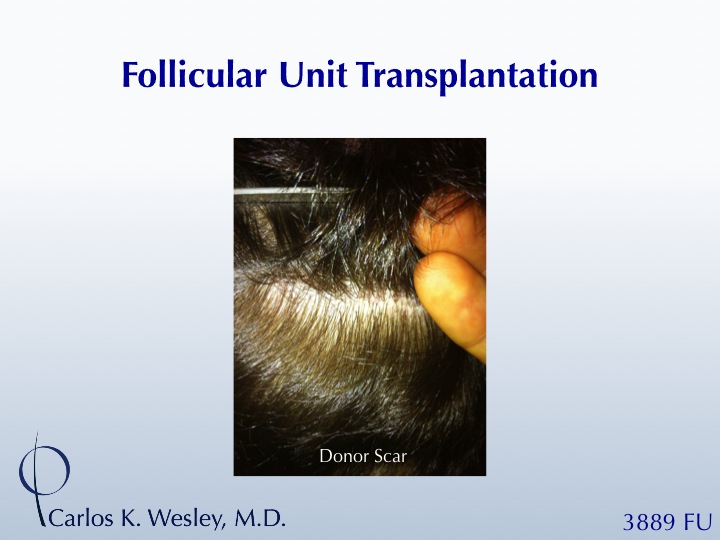
This case was an FUT session. I have attached an image of the patient's resultant donor scar. It's helpful to see a comparison between parting the hair where there is no scar versus parting it along the donor scar.
I'll be sure to have our office post more FUE cases as well.
Spanker, most of our patients come from referrals from MDs and hairstylists rather than from online. This may be a reason for why you don't see as many online postings from my patients as they often aren't aware of these sites. I'll be sure to "nudge" a few as the year goes on, however, to have them share their experiences.
-
Thanks for your comments.
He also suffered from virtually no shock loss during his postoperative process. While this is something we warn our patients of who have considerable pre-existing hair in the recipient area (my practice encourages patients to keep their hair at its normal length for FUT sessions so that they may return to work or social activities sooner), it tends to be much more common in female patients than in male patients.
-
Thanks for the comments, everyone.
Spanker: Miniaturized hairs have a diameter less than 0.03mm while terminal hairs are larger hairs with a diameter exceeding 0.06mm and a length greater than 1cm. These numbers probably aren't going to be that helpful, however, for the average person inspecting their hair in the bathroom mirror. So, I do consider miniaturized hairs in patients relative to their normal, terminal hair shaft caliber. There are plenty of patients with finer caliber hair that are still great candidates if their donor hair consists of a very small percentage in miniaturized form.
BrianR: With respect to a patient's candidacy, I am only referring to miniaturized hairs in their donor area. Good candidates will have plenty of miniaturized hairs in their recipient area because that is the area that has and will continue to thin. It is the long-term survival of donor hair that is being transplanted into that area that matters (as well as the careful planning and placement of those hairs into the recipient region).
-
Thanks, chrisdav and Future_HT_Doc. The chapter's in print as of last week!
fueonly: It's unfortunate that you were not made aware of the likelihood of hypo-pigmentation and punctate scarring prior to you FUE session. "Invisible" is a term akin to "always" and "never" that does not have much of a place in medicine based on the methods used today. Perhaps the best thing that you can do to make other patient's aware of your experience is to describe it and post images of your recovery after the process (on that separate forum that Future suggested) so that other patients with your skin type may have a more accurate idea as to what to expect.
Regarding medical boards: the American Board of Hair Restoration Surgery (ABHRS) is the certifying body specific to our field.
-
Two of the questions posed to me prior to presenting the details of Pilofocus' graft harvesting technique are: 1) how do we evaluate growth of transplanted grafts and 2) how is it done objectively and in a blinded fashion? This is not overly challenging when conducted within a bald area. But what if patients in the clinical trial would like to camouflage the grafts within their pre-existing hair?
Two interactive links below illustrate this method of determining viability of transplanted grafts within a hair-bearing area. Hair viability analyses are performed in a double-blind manner. Therefore, the type of graft transplanted (FUE, FUT, or Piloscopic) is unknown to the observer. Software enables subtle adjustment of each image relative to the other (not possible here). Therefore, near-perfect alignment of hair shafts can be produced to most accurately quantify the presence or absence of transplanted hair when the patients return for follow-up evaluation.
Interactive Example #1 (superimposed before/after sans sites)
Interactive Example #2 (with based on recipient sites)
Go ahead and give counting a try. I can incorporate the results of this poll in the presentation that we have been invited to deliver at the upcoming ISHRS Meeting in San Francisco, CA next month!
-
Thanks, CaddyTad77. Yes. I remember speaking with you and I'll answer you offline.
Our engineering team is designing the next iteration of the device that we plan to test in a few weeks and display during October's ISHRS meeting. Later this week I will post images of the a few results so that members can get a sense of how we quantify growth of newly transplanated hairs. It's all pretty exciting!
-
Patients often come into an office wondering whether or not they are "good candidates" for surgical hair restoration. Even when told "yes" or "no" by the physician, a patient may want to better understand why they are or are not deemed a good candidate and where he or she may fit into the overall spectrum of candidacy.
While young patients can certainly refer to a helpful publication authored by our practice (view here) that helps provide a ballpark for the ultimate number of donor hairs one may anticipate over their lifetime, it is helpful to know about the "miniaturization" rule. Using magnified images of a patient's donor hair, a physician can determine the number of miniaturized hairs (those of the finest caliber compared to the regular caliber terminal hairs). As a general rule of thumb, young patients who possess 25% or more of their donor hair in miniaturized form are not great candidates for the surgical procedure. Not only will a large number of the transplanted hairs likely not be permanent hairs, but also the donor scarring (either FUT or FUE) will likely become exposed over time if the surrounding donor hair continues its anticipated course of MPB.
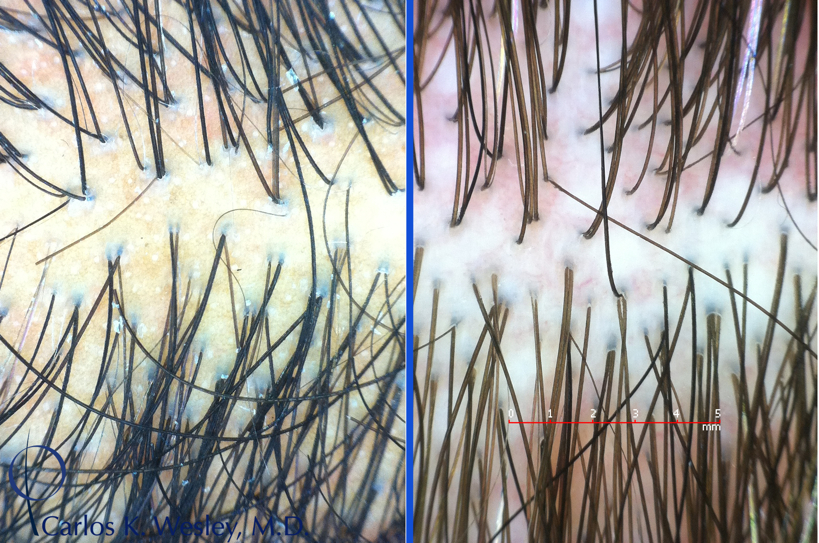
The following image depicts a relatively poor candidate for HRS on the left and a better candidate for HRS on the right. This is based on the relatively low number of miniaturized hairs present in the righthand patient's donor area. Both were of the same age.
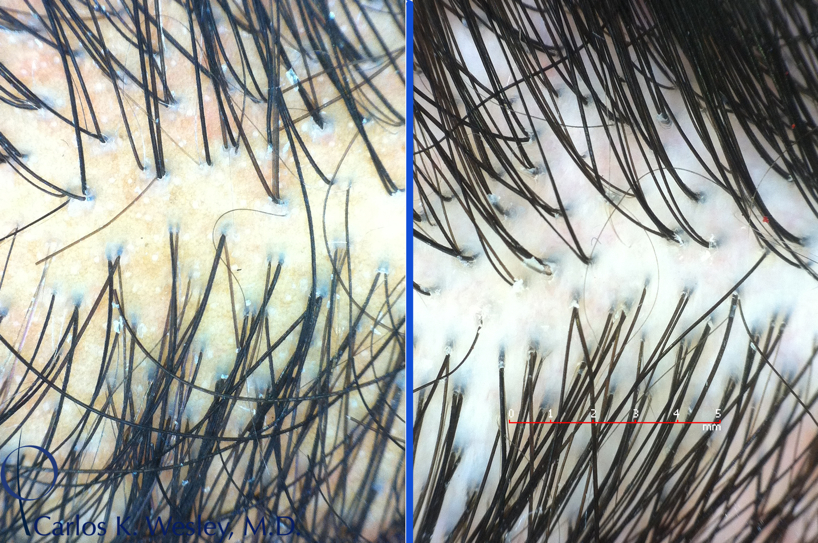
This next image also compares a poor candidate (left) with a much better candidate for the procedure (right).
There are also a number of more subjective variables that help determine a patient's candidacy: the wave, curl, frizz, and color contrast between the hair and scalp. These can also influence the ultimate appearance of a patient after a full session.
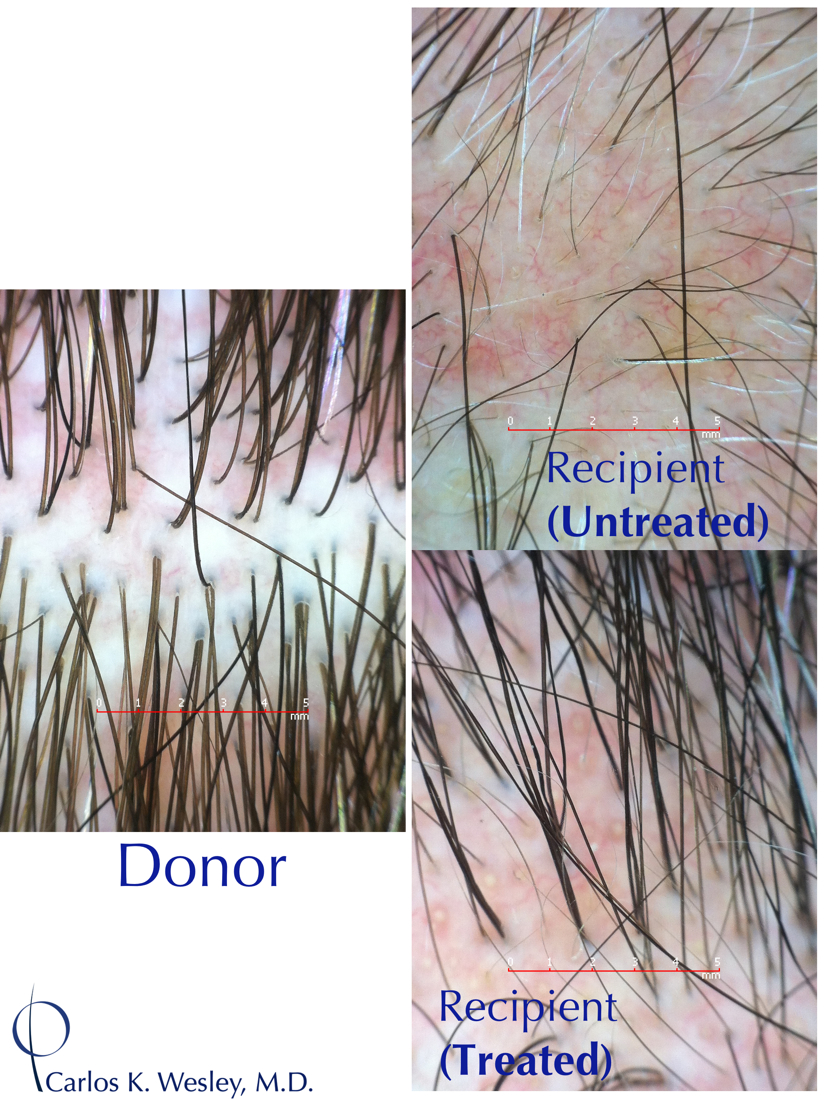
To put it all together, here is an image of a good candidate's donor area, recipient area prior to treatment, and his recipient area after treatment as seen under a magnified lens. The same patient's transformation after a 2701-graft FUE session with me can be viewed in the accompanying video montage.
-
 1
1
-
-
This patient recently returned to our office to display his donor scar after two strip harvest session totaling 4020 grafts. We've been able to update his complete transformation video (seen earlier in this thread) as well as addinghttp://vimeo.com/73333653 below that is specifically focused on his donor scar.
-
Thanks, Spanker and agenteye, for your comments.
That's the correct nomenclature, Future_HT_Doc! Since the sessions involving very large "plugs" are essentially obsolete, the term follicular unit transplantation (FUT) has taken on a new form. Now that follicular unit extraction (FUE) so clearly, specifically, and effectively refers to the idea of harvesting individual follicular units one at a time directly from the donor area, any other reference to FUT is generally assumed to be strip harvest.
It's true that FUSS is a more specific term and should probably be used to more specifically describe the manner of graft harvest.
-
During my recent trip to Boston to see new consult patients, I also had previous surgical patients drop by. Here is an image of this patient taken approximately two (2) years after his session. While I didn’t travel with our NYC office’s best camera or have our ideal lighting, you can still get a sense of his new facial framing from the procedure.

I’ve also included an updated image of his donor scar from follicular unit transplantation (FUT).
-
I’ve also included an image of his donor scar from follicular unit transplantation (FUT).
-
1) What are FFs?
2) Are 3s the largest size graft you use?
3) Can you illustrate how you distribute these grafts throughout the scalp (for example, in Mickey85's post diagraming FU placement only 1s are used in the front of the scalp - is that your approach as well?):
- Nathaniel
FFs are Follicular Families. They involved four (4) or more hair follicles and are found in patients with relatively dense and closely-packed bundles of hair. They are great for density, but not for a soft hairline. It's best to use them behind a series of fine 1-haired grafts that are blended with fine 2-hair grafts. There is always a general progression of more "full" grafts (those with a larger number of hairs/graft) when you work your way posteriorly (backwards) from the hairline as well as a progression of finer caliber hair to more coarse caliber hair. This helps generate a more natural gradient of softness to fullness.
It varies, however, in patients who have minimal color contrast between their hair and scalp (surgeons can more readily add more "full" grafts closer to the hairline) versus patients who have greater color contrast between their hair and scalp (in whom the more "full" grafts are best tucked behind more fine-caliber follicles).
-
This patient has been known to our office for many years. He began taking finasteride about four years ago. In addition, he had been coupling this with topical minoxidil 5% for three years prior to any surgical intervention.
At only 7 months, I encouraged our office to display this montage, not for the recipient growth (which will continue and you will see from all angles once it's grown in fully), but rather to illustrate the planning process in a young man. In our office's peer-reviewed publication that compiled the opinions of 34 of the world's most experienced hair restoration surgeons worldwide with nearly 1000 years of combined experience, there's a limit to the amount of safe donor scalp hair that can be harvested.
The key points that I feel strongly about (and you may see differently) are:
- having this young patient really commit to medical treatment and seeing it's benefit before undergoing FUT or FUE;
- creating a cosmetic improvement that doesn't draw attention to itself (donor and recipient), but rather gives that patient a healthier look; and
- ensuring that the pattern will continue to be age appropriate in his 40s, 50s, etc.
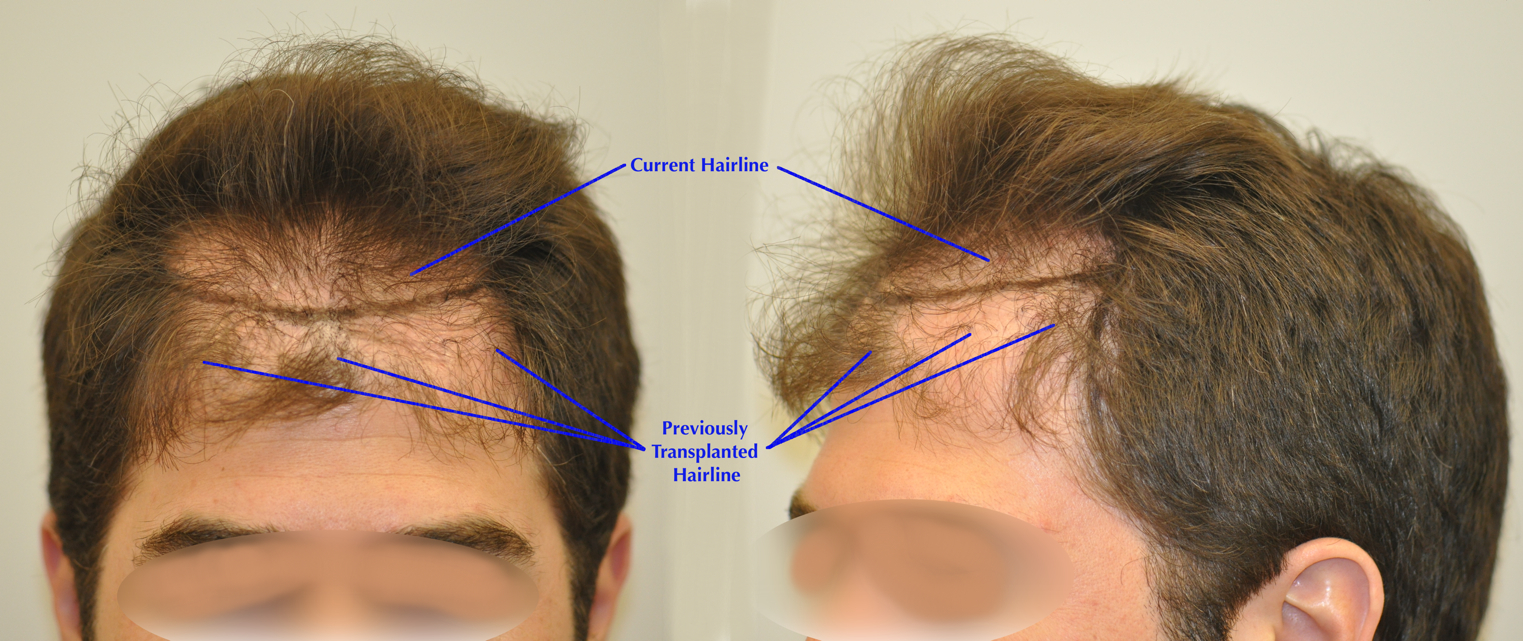
You can see how low this 23-year-old athlete's existing hairline currently was. Giving in to the temptation to transplant at that level would have resulted in the type of unnatural outcome (see pic below) that I've seen from patients coming in for repairs after having that overly-aggressive hairline treatment performed by other HT clinics at a patient's young age. The transplanted pattern simply doesn't match what nature had intended. It's important for a patient to look great 18 months after the procedure when the transplanted hair has fully grown in. It's equally important for them to look great 18+ years after their session when their pre-existing hair has continued to recede.
- having this young patient really commit to medical treatment and seeing it's benefit before undergoing FUT or FUE;
-
For those interested, I have attached a video that demonstrates the surgical technique involved in performing a trichophytic closure for FUT cases. It differs from a standard surgical closure in that the edge (either one or both) of the donor wound is first "prepped" (i.e. a 1mm portion is removed from the surface) before the closure is performed. Carefully bringing the newly-formed edge together with the opposing donor edge enables hair to grow through the donor scar. This helps further camouflage the donor scar.
Caveat emptor: This may not be video for those with queazy stomachs. Enjoy!
-
Here's an update on this patient who underwent a session to the front and also the mid scalp region. While high density of transplantation is often a strong point of emphasis on this forum, it's not always the most appropriate approach.
This patient desired a soft, natural-appearing coverage of his scalp with a virtually imperceptible donor scar. So, his treatment plan was designed to bring his coverage back to the vertex transition point (where the head begins to slope downwards). Often times, leaving an untreated crown while adding hair coverage around it is one of the most effective ways to generate a more natural-appearing transplant.
-
You're very welcome. I prefer the blunt 0.8mm punch as, in my hand, I find that it tends to minimize transection (versus sharp punch).
My preference is also to limit FUE sessions to <2000 grafts/day. The out-of-body time for these types of grafts that do not possess as much protective surrounding subcutaneous tissue as those from a strip harvest can start to impact their survival after many hours.
-
We're certainly looking at it closely and have effectively adopted the use of both Acell and PRP into our patients' FUE donor healing. Although we haven't initiated any formal investigation, there is anecdotal evidence that it can help regenerate hair follicles from transacted hair fragments in the donor area.
-
Thanks for your comments.
The song is "Sweet Disposition" by The Temper Trap.
We learn all sorts of wonderful things on this site!
-
Wherever your HT was performed, that is certainly a wider than average scar, xtactic5. Good thing is that, at only four months post-op, the redness will continue to subside a bit. I agree with gillenator that you should contact your doctor's office to find out the details as it will inform you and help you plan in the future.
A focused scar reduction or FUE into the residual donor scar can certainly help camouflage it down the road and allow to to comfortably wear your surrounding donor hair at a much shorter length.
-
At long last, this article just came out in print in the May 2013 edition of the peer-reviewed journal Dermatologic Surgery.
I think another 1000 grafts via FUE is a reasonable estimate, Spanker. In addition, if you begin to include grafts harvested from the beard via FUE, you can increase that number considerably...














Carlos K. Wesley, M.D. (NYC): Focused Mid Scalp on Young Male
in Results Posted by Leading Hair Restoration Clinics
Posted
Thanks for your comments.
@irishsailor, this patient certainly has the option of coming back down the road to treat his crown and even add to the previously-untreated frontal portion if he wishes. The advantage is that he won't be obligated to do this in order to maintain a natural appearance as his inevitable course of MPB continues over time. This transplant design can serve as both a conservative eventual hairline as well as being consistent with the arc of a thinning crown.
As you well know, focusing on the crown exclusively in a young patient may ultimately result in an unnatural "island" of hair over time as his MPB takes its course and the surrounding hair thins.